Klebsiella is a genus of bacteria that has garnered attention in recent years due to its role in various infections, particularly in hospital settings. This article explores the characteristics, pathogenicity, transmission, diagnosis, treatment, and prevention of Klebsiella infections, shedding light on its significance in public health.
What is Klebsiella?
Klebsiella is a genus of Gram-negative bacteria belonging to the family Enterobacteriaceae. It comprises several species, with Klebsiella pneumoniae being the most clinically relevant. Other notable species include Klebsiellas oxytoca and Klebsiellas rhinoscleromatis. Klebsiellas species are opportunistic pathogens, meaning they can cause infections primarily in individuals with weakened immune systems or underlying health conditions.
Klebsiella bacteria are commonly found in the environment, particularly in soil, water, and the intestines of humans and animals. They are rod-shaped, non-motile, and often encapsulated, which enhances their virulence. The capsule serves as a protective barrier against the host’s immune system, facilitating the bacteria’s ability to cause disease.
Pathogenicity of Klebsiella
Klebsiella pneumoniae is primarily known for causing pneumonia, but it can also lead to a range of other infections, including urinary tract infections (UTIs), bloodstream infections, and infections of wounds and surgical sites. The pathogenicity of Klebsiella is attributed to several factors:
1. Capsule Formation
The thick polysaccharide capsule of Klebsiella protects it from phagocytosis by immune cells, allowing the bacteria to survive and multiply in the host.
2. Adhesion Factors
Klebsiella possesses various surface adhesins that enable it to adhere to host tissues and evade the immune response, leading to infection.
3. Production of Virulence Factors
Klebsiella produces several virulence factors, including enzymes like mucinase, which helps in tissue invasion, and siderophores, which facilitate iron acquisition from the host, promoting bacterial growth.
4. Antibiotic Resistance
A growing concern in Klebsiella infections is the emergence of antibiotic-resistant strains. Many strains have developed resistance to multiple antibiotics, including extended-spectrum beta-lactamases (ESBLs) and carbapenemases, making treatment increasingly challenging.
Transmission of Klebsiella
Klebsiella infections are primarily associated with healthcare settings, where transmission often occurs through:
- Direct contact with contaminated surfaces or healthcare personnel.
- Invasive procedures, such as catheterization or surgery, which can introduce the bacteria into sterile areas of the body.
- Person-to-person transmission, particularly in environments with high patient turnover and close proximity, such as hospitals and nursing homes.
The bacteria can also be found in the community, where they can cause infections in individuals with risk factors, such as diabetes, chronic lung disease, or recent antibiotic use.
Clinical Manifestations
Klebsiella infections can manifest in various ways, depending on the site of infection:
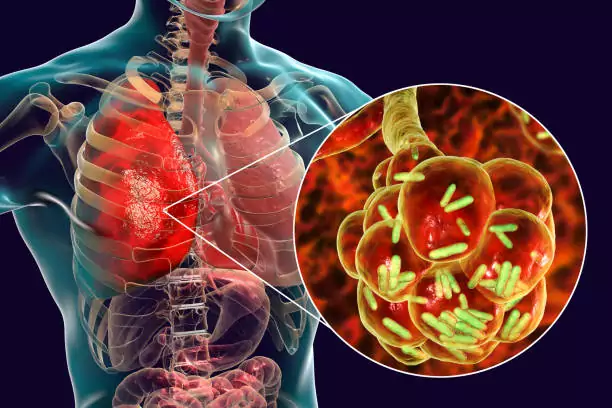
1. Pneumonia
Klebsiella pneumonia is a severe lung infection characterized by cough, fever, chills, and difficulty breathing. It often presents with thick, mucoid sputum that may be blood-tinged.
2. Urinary Tract Infections
Klebsiella is a common cause of UTIs, especially in individuals with urinary catheters. Symptoms may include dysuria, urgency, and flank pain.
3. Bloodstream Infections
Klebsiella bacteremia can occur, particularly in hospitalized patients, leading to sepsis. Symptoms may include fever, chills, and signs of organ dysfunction.
4. Wound and Soft Tissue Infections
Infections can arise from surgical wounds or trauma, leading to cellulitis, abscess formation, or necrotizing fasciitis in severe cases.
Diagnosis of Klebsiella Infections
Diagnosis of Klebsiella infections typically involves:
1. Microbiological Culture
Specimens such as sputum, urine, blood, or wound swabs are collected and cultured to identify the presence of Klebsiella. Isolation of the bacteria allows for further testing, including susceptibility testing to determine antibiotic resistance patterns.
2. Molecular Methods
Polymerase chain reaction (PCR) and other molecular techniques can provide rapid identification of Klebsiella and detect specific resistance genes.
3. Imaging Studies
In cases of pneumonia or abscess formation, imaging studies such as chest X-rays or CT scans may be employed to assess the extent of the infection.
Treatment of Klebsiella Infections
The treatment of Klebsiella infections depends on the site and severity of the infection, as well as the susceptibility of the isolated strain. Common treatment strategies include:
1. Antibiotic Therapy
Empirical antibiotic therapy is often initiated based on local resistance patterns. Commonly used antibiotics include:
- Beta-lactams (e.g., ceftriaxone, cefotaxime) for susceptible strains.
- Carbapenems (e.g., meropenem, imipenem) for resistant strains.
- Aminoglycosides (e.g., gentamicin) may be used in combination therapy for severe infections.
2. Supportive Care
In addition to antibiotics, supportive care is crucial, especially in severe cases. This may include oxygen therapy, intravenous fluids, and monitoring of vital signs.
3. Surgical Intervention
In cases of abscess formation or necrotizing infections, surgical intervention may be necessary to drain infected fluid or debride necrotic tissue.
Prevention of Klebsiella Infections
Preventing Klebsiellas infections involves several strategies, particularly in healthcare settings:
1. Hand Hygiene
Strict hand hygiene practices among healthcare personnel and visitors can significantly reduce the risk of transmission.
2. Environmental Cleaning
Regular cleaning and disinfection of surfaces and equipment in healthcare facilities can help eliminate potential sources of infection.
3. Antibiotic Stewardship
Implementing antibiotic stewardship programs to promote appropriate antibiotic use can reduce the emergence of resistant strains.
4. Infection Control Measures
Utilizing isolation precautions for patients infected or colonized with Klebsiellas and ensuring the proper use of personal protective equipment (PPE) are essential in preventing outbreaks.
5. Vaccination
While no specific vaccine for Klebsiellas exists, vaccines targeting other respiratory pathogens may indirectly reduce the incidence of Klebsiellas pneumonia by preventing concurrent infections.
Conclusion
Klebsiella is a significant pathogen in both healthcare and community settings, with the potential to cause severe infections. Understanding its characteristics, pathogenic mechanisms, and the challenges associated with antibiotic resistance is crucial for effective prevention, diagnosis, and treatment. Ongoing surveillance and research are essential to combat the threat posed by Klebsiellas and ensure better outcomes for affected patients. As healthcare providers, patients, and the public become more aware of Klebsiellas and its implications, the focus can shift toward improving infection control measures and antibiotic stewardship to mitigate the impact of this opportunistic pathogen.